Overview: Think your heartburn is harmless? Learn the warning signs your reflux may indicate GERD or a more serious condition that needs expert care!
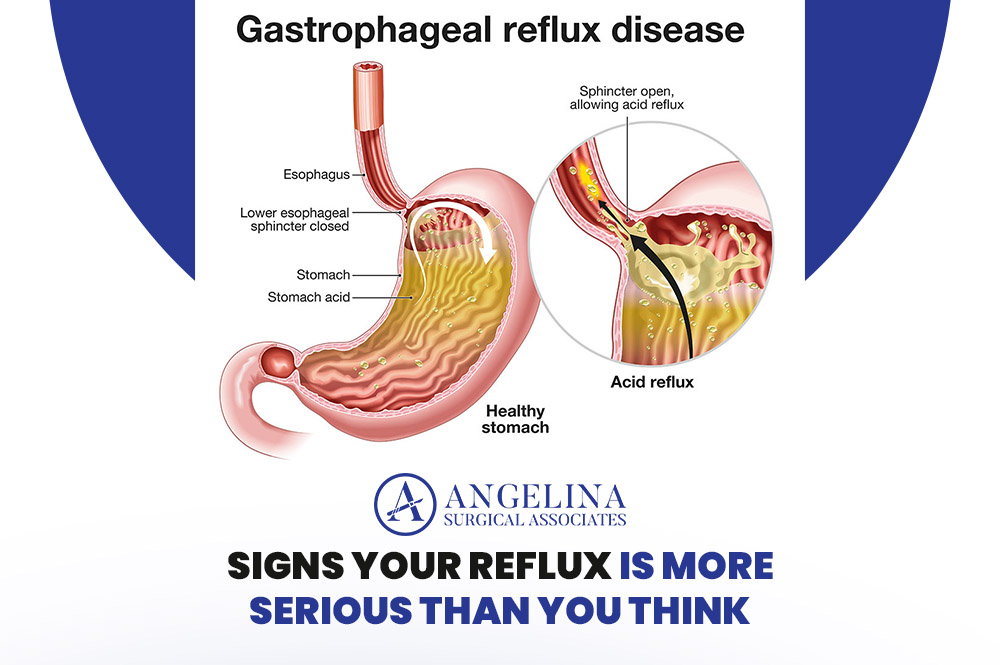
If you’ve ever felt that familiar burning sensation after a heavy meal or late-night snack, you’re not alone. Gastroesophageal reflux disease (GERD) and acid reflux are incredibly common, but not all reflux is the same. For some people, those symptoms may point to something more serious — something that requires medical attention rather than just an over-the-counter antacid.
As a surgical specialist who sees patients with reflux-related complications regularly, we can tell you that recognizing when reflux crosses the line from “occasional nuisance” to “chronic condition” can make all the difference in protecting your long-term health.
Let’s get into it for more!
1. Your Symptoms Are More Frequent or Severe
Occasional heartburn after spicy food or coffee is normal. But when symptoms occur more than twice a week or begin to interfere with sleep, appetite, or daily activities, it’s no longer simple reflux — it’s likely GERD.
Chronic acid exposure can damage the lining of your esophagus over time, leading to inflammation, scarring, or even precancerous changes known as Barrett’s esophagus. That’s why persistent reflux should never be brushed aside or self-treated indefinitely.
2. You’re Experiencing Difficulty Swallowing or Pain When Swallowing
If you find yourself avoiding certain foods, needing extra water to swallow, or feeling like food “sticks” on the way down, it could signal esophageal narrowing caused by ongoing inflammation. In some cases, this can also point to a more advanced condition.
While it may start subtly, progressive difficulty swallowing (known as dysphagia) warrants immediate evaluation. Early intervention can prevent complications and improve your quality of life.
3. You’ve Developed Chronic Cough or Hoarseness
Reflux doesn’t always show up as heartburn. In fact, some patients have what’s known as “silent reflux” — where acid travels high enough to irritate the throat, voice box, or even the airways without causing obvious chest discomfort.
If you’ve had a lingering cough, a hoarse or raspy voice, or frequent throat clearing without an apparent cause, reflux could be to blame. ENT specialists and gastroenterologists often work together to identify and manage these cases effectively.
4. You’re Waking Up at Night With Burning or Choking Sensations
When reflux becomes severe, stomach acid can backflow while you’re lying down, causing sudden episodes of choking, coughing, or shortness of breath at night.
These nocturnal symptoms are more than uncomfortable — they’re a red flag that acid is reaching higher into your esophagus and possibly your airways.
Persistent nighttime reflux not only disrupts sleep but can also lead to respiratory problems if untreated.
5. You’ve Tried Lifestyle Changes and Medications Without Relief
Avoiding trigger foods, eating smaller meals, elevating your head at night, and using medications like proton pump inhibitors (PPIs) can help most people with mild reflux. But if you’ve been following these steps and still experience symptoms, that’s a sign it’s time to dig deeper.
Chronic reflux that resists medical therapy could mean your lower esophageal sphincter (LES) — the valve between your stomach and esophagus is weakened or not functioning properly. In such cases, surgical or minimally invasive procedures, such as the LINX procedure or fundoplication, may offer long-term relief and prevent further damage.
Know When to Seek Professional Help
If your reflux symptoms have become routine, severe, or are accompanied by any of the warning signs above, it’s important to consult a specialist. At Angelina Surgical, we evaluate not just your symptoms, but the underlying causes.
Using tools such as endoscopy, pH monitoring, and imaging studies, we determine the extent of the problem and create a personalized treatment plan — whether that involves medication management, lifestyle guidance, or minimally invasive surgical options.
You don’t have to live with discomfort, disrupted sleep, or worry about long-term damage. Early diagnosis and the right treatment approach can help you regain control over your digestive health and your life.